This content is archived from the Feline Nutrition Foundation
Answers: Cats in a Bind over Phosphorus
- Updated: Monday, May 06, 2019 12:26 PM
- Published: Saturday, September 12, 2015 07:21 PM
- Written by Elisa Katz, DVM
 My cat is in the early stages of kidney disease. My vet said he wanted to reduce her phosphorus intake. Since I don't like the prescription diets and my cat, who eats a raw cat food diet, wouldn't touch them anyway, what are my options to accomplish a reduced phosphorus diet?
My cat is in the early stages of kidney disease. My vet said he wanted to reduce her phosphorus intake. Since I don't like the prescription diets and my cat, who eats a raw cat food diet, wouldn't touch them anyway, what are my options to accomplish a reduced phosphorus diet?
Phosphorous is present in most foods, but meat and dairy tend to have the most. When serial blood testing reveals that a cat has declining kidney function, called renal insufficiency, phosphorous should be somewhat restricted to decrease the risk of one of the major long term effects of kidney insufficiency, secondary hyperparathyroidism. For the most part, this can be achieved easily through dietary changes. In later stages, phosphorus binders may be indicated. Dietary modification is an important way to help control phosphorus. However, commercial feline renal diets typically restrict phosphorus by using reduced amounts of protein. Unfortunately, in addition to lower amounts of this vital nutrient, these diets also typically use cheaper, lower-quality proteins and make up for the lost calories by adding fillers. These diets may improve a cat's blood test results, but they often result in muscle wasting due to a lack of sufficient protein to maintain the muscle mass in this obligate carnivore.
 So, what do phosphate binders do? Phosphate binders prevent absorption of phosphorus consumed in the diet as well as bind phosphorus present in bile, saliva and intestinal secretions. Historically, aluminum hydroxide was commonly used. However, recent research has demonstrated that persistent consumption of an aluminum-containing product can be toxic to ailing kidneys.¹ Therefore, this product has fallen out of favor. Other phosphate binders include calcium carbonate, calcium acetate, sevalamar HCL and lanthanum carbonate. The aforementioned products are either yucky-tasting liquids or pills that most cats will not take easily. A newer, easier to administer, though somewhat less potent phosphate binder called Epakaitin® is available and is a good choice to use early in the course of renal insufficiency.² It comes as a flavored powder that can be mixed with food.
So, what do phosphate binders do? Phosphate binders prevent absorption of phosphorus consumed in the diet as well as bind phosphorus present in bile, saliva and intestinal secretions. Historically, aluminum hydroxide was commonly used. However, recent research has demonstrated that persistent consumption of an aluminum-containing product can be toxic to ailing kidneys.¹ Therefore, this product has fallen out of favor. Other phosphate binders include calcium carbonate, calcium acetate, sevalamar HCL and lanthanum carbonate. The aforementioned products are either yucky-tasting liquids or pills that most cats will not take easily. A newer, easier to administer, though somewhat less potent phosphate binder called Epakaitin® is available and is a good choice to use early in the course of renal insufficiency.² It comes as a flavored powder that can be mixed with food.
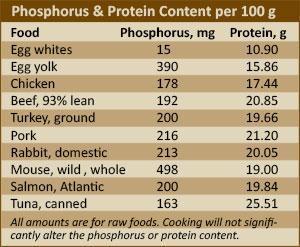
One fairly easy and effective way to reduce the overall phosphorus in a cat's diet without sacrificing protein is to feed cooked egg whites. Egg whites contain much less phosphorus per gram of protein than other protein-rich foods such as meats or fish.³ For instance, 100 grams of egg white, which is approximately 3 egg whites or 3.5 ounces, will contain 10.9 g of protein and only 15 mg phosphorus. Compare this to 100 g of ground chicken, which contains 17.44 g protein, but has 178 mg phosphorus. The same 100 g of salmon contains 19.84 g protein and 200 mg phosphorus. If we calculate a ratio for each of these, we can see that the phosphorus/protein ratio for egg whites is far lower than for other protein sources. To reduce phosphorus without restricting protein, you could replace 33 g of meat, a bit over one ounce, with one cooked egg white. Your cat would be consuming considerably less phosphorus in that portion. In fact, a study in humans found that 92% of dialysis patients were able to lower their serum phosphorus levels significantly by replacing 8 ounces of meat in their diet with egg whites.⁴
Renal secondary hyperparathyroidism can result from long-term excess of phosphorus. In addition to making a patient feel ill, elevated phosphorus results in decreased blood calcium levels, because calcium and phosphorus must be kept in delicate balance. Over time, the parathyroid glands release a hormone that leaches calcium out of the bones to replace it in the bloodstream and avoid problems associated with low blood calcium. This results in soft, fragile bones, possible fractures and mineral deposits in various organs, including the kidneys.⁵
Additional Reading
Answers: Feed My Cat a Raw Egg Yolk?
Phosphorus Can Be Key for Cat Kidneys
The bottom line is that we know cats are obligate carnivores and have higher protein requirements than other species. Research has shown that in the early stages of renal insufficiency, limiting protein can result in decreased blood reaching the kidneys and may actually be worse than feeding moderate amounts of protein.⁶ Until your cat's blood kidney values are progressively worsening, something such as Epakaitin® is an easy to use, affordable product and one that I have used with much success. Remember, cats with this condition need to be monitored at least every six months, possibly more frequently. You need to discuss your cat's condition with your veterinarian to determine what is ideal for your cat.
Note: Feline Nutrition provides feline health and nutrition information as a public service. Diagnosis and treatment of specific conditions should always be in consultation with your own veterinarian. Feline Nutrition disclaims all warranties and liability related to the veterinary advice and information provided on this site.
Dr. Elisa Katz, DVM, is a graduate of Ohio State University and is the owner of Natural Pet Animal Hospital in Bourbonnais, Illinois. She practices holistic and integrative medicine focusing on proper diet and nutrition. Dr. Katz shares her home with four kitties and one dog.
1. DC Chew, "Chronic Kidney Disease (CKD) in Dogs & Cats - Staging and Management Strategies," Virginia Veterinary Conference Presentation, Virginia Veterinary Medical Association, 2015.
2. "Epakitin and Azodyl Clinical Studies," Vetoquinol USA, 2008-2009.
3. USDA National Nutrient Database for Standard Reference, Release 28, September 2015.
N. Wille, "Reinventing the Mouse – Nutritional Analysis of Mice," TCFeline, 2010.
4. JA Charnow, editor, "Egg Whites May Help Lower Phosphorus," Renal and Urology News, May 1, 2008.
5. SJ Ettinger and E Feldman, Textbook of Veterinary Internal Medicine, 4th ed., WB Saunders, Philadelphia, PA, 1995.
6. GF Grauer, "Slowing the Progression of Chronic Renal Failure," Kansas State University, Department of Clinical Sciences.




