This content is archived from the Feline Nutrition Foundation
Feline Hyperthyroidism: What You Need to Know
- Updated: Monday, April 29, 2019 03:33 PM
- Published: Saturday, May 26, 2012 10:54 AM
- Written by Guillermo Díaz. MV
 Hyperthyroidism, or thyrotoxicosis, is the most common endocrine disease in cats. When an animal or a person has hyperthyroidism it means that there is a high concentration of thyroid hormones in the blood. The opposite, low thyroid hormone levels, is called hypothyroidism. Hyperthyroidism occurs mostly in older cats, generally around 12 years old, although reports have shown a wide range between 4 and 23 years.¹ There is no predisposition related to sex or breed.
Hyperthyroidism, or thyrotoxicosis, is the most common endocrine disease in cats. When an animal or a person has hyperthyroidism it means that there is a high concentration of thyroid hormones in the blood. The opposite, low thyroid hormone levels, is called hypothyroidism. Hyperthyroidism occurs mostly in older cats, generally around 12 years old, although reports have shown a wide range between 4 and 23 years.¹ There is no predisposition related to sex or breed.
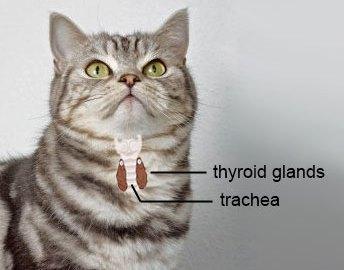
The thyroid gland is a thin structure located in the neck, and consists of two lobes lying on each side of the trachea. In humans, it is connected by a narrow band of tissue called the isthmus. In cats, the isthmus is vestigial, resulting in two separate lobes. The thyroid glands regulate the speed at which your cat's metabolism works through the production of thyroid hormones, much like the accelerator regulates the speed of your car. It regulates the speed of all body processes: kidney and liver function, brain, digestive system, skin, etc. When too much of the hormone is produced, the cat has become hyperthyroid.
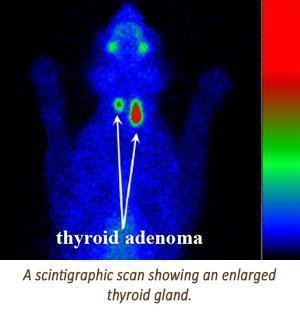
There are two basic causes for the over-production of thyroid hormone. The first and most frequent, accounting for around 98% of cases, is adenomatous hyperplasia. This is the enlargement of the functional normal tissue, and is bilateral in around 70% of cases. The second cause of high levels of thyroid hormone is thyroid carcinoma or cancer. This type of presentation is rare, accounting for no more than 2% of cases.²
 What causes the thyroid to malfunction in the first place? For decades, doctors and scientists have tried to answer this question. New technology may be providing an answer. EPA research biologist Janice Dye has concluded that chronic exposure to certain chemicals, called polybrominated diphenyl ethers, may explain hyperthyroid disease in older cats.³ These chemicals interact with thyroid-binding proteins to displace thyroxine. Chronic exposure may lead to thyroid hyperplasia. Cats can ingest PBDEs in certain foods or by licking PBDEs-laden house dust from their fur. Fish-flavored brands of canned cat food can contain high levels of PBDEs. Also, PBDEs are commonly used as flame-retardants in fabrics and other household items.⁴ Cat owners should determine whether their blankets and bedding for cats are PBDEs-free.
What causes the thyroid to malfunction in the first place? For decades, doctors and scientists have tried to answer this question. New technology may be providing an answer. EPA research biologist Janice Dye has concluded that chronic exposure to certain chemicals, called polybrominated diphenyl ethers, may explain hyperthyroid disease in older cats.³ These chemicals interact with thyroid-binding proteins to displace thyroxine. Chronic exposure may lead to thyroid hyperplasia. Cats can ingest PBDEs in certain foods or by licking PBDEs-laden house dust from their fur. Fish-flavored brands of canned cat food can contain high levels of PBDEs. Also, PBDEs are commonly used as flame-retardants in fabrics and other household items.⁴ Cat owners should determine whether their blankets and bedding for cats are PBDEs-free.
Symptoms to Look For
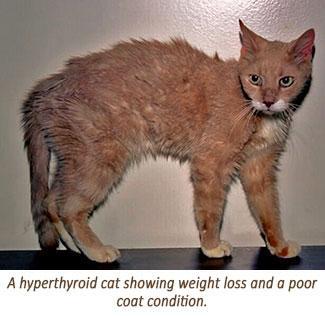
Most cats show an enlargement of the thyroid gland and weight loss, despite an increase in appetite and intake of food. This is generally the first and most common symptom an owner would see. Due to the effect of the hormone in the brain, cats affected usually become more energetic and hyperdynamic. In some cases, nervousness and even aggression towards owners may be present. Some cats show muscle weakness, diarrhea and increased volume of feces due to the increased food intake. There might be other symptoms, such as poor coat condition, increased heart rate, increased urination, heart murmurs, vomiting, lethargy, increased respiratory rate or tremors. There can be more than one symptom in a cat, and the intensity may vary amongst individuals.
Testing for Hyperthyroidism
The veterinarian will test a cat's blood as part of the process to rule out or confirm the disease. There are several indicators which may suggest hyperthyroidism, but measuring the level of the thyroid hormone is the best test. The tests commonly used are the measurement of thyroxine, which is often abbreviated as T4, and a T3 suppression test. Normal T4 ranges in cats vary from 12.87 nmol/L to 38.61 nmol/L.
 Another test is the scintigraphic scan. Radioactive iodine is given to the cat in very small doses. The compound is then transported by the blood to the thyroid glands. Hyperfunctional thyroid glands accumulate more of the compound than normal glands, which can be easily scanned and measured. Scintigraphic scans are often used to confirm the diagnosis after a blood test indicates the cat may be hyperthyroid.
Another test is the scintigraphic scan. Radioactive iodine is given to the cat in very small doses. The compound is then transported by the blood to the thyroid glands. Hyperfunctional thyroid glands accumulate more of the compound than normal glands, which can be easily scanned and measured. Scintigraphic scans are often used to confirm the diagnosis after a blood test indicates the cat may be hyperthyroid.
Treating Hyperthyroidism
Your doctor has different options for treating this disease, such as anti-thyroid drugs, surgery and radiation. The prognosis for cats affected is very good as long as the owner complies with periodic checkups.
The most commonly used drugs are methimazole and carbimazol. The first is most commonly used in the United States, and is very effective in controlling the disease by blocking the synthesis of thyroid hormone. This means that methimazole does not destroy abnormal adenomatous thyroid tissue. This treats but doesn't actually cure the illness. The most common transient side effects are vomiting, anorexia, lethargy and blood disorders. Cats under drug treatment must have their blood checked for T4 levels and other values such as liver, kidney and CBC. This must be done every two to three weeks at the beginning of treatment in order to adjust dosage until the patient reaches an acceptable T4 value of 10 - 25 nmol/L.
There are procedures that do cure hyperthyroidism: surgery and radiation treatment. The candidates for these procedures must meet certain criteria. They must be younger or middle age patients with mild hyperthyroidism. This means that they have not developed complications related to chronic hyperthyroidism. Also, they must not suffer from non-thyroid related diseases, such as renal insufficiency or heart problems.
Surgery involves removing the thyroid entirely. When cats remain hyperthyroid after surgery, they probably have thyroid tissue in abnormal locations, such as inside the thorax, where removal is difficult. These cats have what is called an ectopic thyroid.
 Radiation treatment is the administration of a radioactive compound, iodine 131, injected endovenously. The thyroid gland naturally takes up iodine, thus the radiation is concentrated there and causes the thyroid to stop working. This is a relatively simple procedure and in most cases does not require the use of anesthesia. The downside of this is that the kitty must remain in the hospital for several days until the radiation has been cleared. This procedure is not offered everywhere because of its cost, the special equipment required and the special training needed.
Radiation treatment is the administration of a radioactive compound, iodine 131, injected endovenously. The thyroid gland naturally takes up iodine, thus the radiation is concentrated there and causes the thyroid to stop working. This is a relatively simple procedure and in most cases does not require the use of anesthesia. The downside of this is that the kitty must remain in the hospital for several days until the radiation has been cleared. This procedure is not offered everywhere because of its cost, the special equipment required and the special training needed.
Hyperthyroidism and Renal Disease
One of the most common complications in cats suffering hyperthyroidism is renal disease. Studies have shown that the prevalence of concurrent hyperthyroidism and renal disease is estimated to be approximately 30 to 35%.⁵ Hyperthyroidism tends to mask symptoms of renal insufficiency because of the increased blood flow through the kidneys. Blood tests can show normal kidney values despite mild to moderate renal disease. When a cat in this stage begins treatment for hyperthyroidism, the blood flow through the kidneys goes back to normal and results in the apparent worsening of the serum kidney function tests. Owners must remember that the treatment of hyperthyroidism itself does not cause kidney disease. The renal problem was already present before treatment, but was masked by the hyperthyroidism.⁶ Cats with renal insufficiency and hyperthyroidism can be challenging to treat. Some doctors want to keep the cat "a little hyperthyroid," in order to help kidney function.
Nutritional Requirements of Hyperthyroid Cats
 As obligate carnivores, cats evolved and adapted all of their systems to eat and digest natural raw diets. Cats have strict requirements for energy from protein and animal fat. If your cat lived in the wild, he would probably chase and eat small animals such as birds and rodents. The content of this prey can be broken down approximately as follows: protein 60-70%, fat 30%, carbohydrates 5-10%.⁷ Note the low levels of carbohydrates in the daily meal of cat living in the wild. This means that cats have very low requirements for carbohydrates. In other words, they don't need them to survive.
As obligate carnivores, cats evolved and adapted all of their systems to eat and digest natural raw diets. Cats have strict requirements for energy from protein and animal fat. If your cat lived in the wild, he would probably chase and eat small animals such as birds and rodents. The content of this prey can be broken down approximately as follows: protein 60-70%, fat 30%, carbohydrates 5-10%.⁷ Note the low levels of carbohydrates in the daily meal of cat living in the wild. This means that cats have very low requirements for carbohydrates. In other words, they don't need them to survive.
The most noticeable symptom of a hyperthyroid cat is weight loss despite an increased appetite. The excess of thyroid hormone has catabolic effects in the feline body. This means that a cat's system "eats" its own muscle tissue in order to meet the increased protein requirements of the new state.⁸ This is why restoring and preserving any remaining muscle tissue in cats treated for hyperthyroidism depends upon the cat consuming a diet with sufficient amounts of high-quality protein. As cats age, they absorb and metabolize protein less efficiently. It's extremely important to feed high-quality protein, i.e., from animal sources rather than grain-based, as well as an adequate quantity of protein.⁹ Grain-based meals, such as dry kibble and some types of canned food, are not appropriate for any cat. They are even more harmful when given to hyperthyroid cats.
Additional Reading
Answers: Goaltending the Cat Food Bowl
High Blood Pressure: Yes, Your Cat Can Get It, Too
Recently, a new prescription commercial diet for treating feline hyperthyroidism has been introduced to the market. Manufacturers state that it contains low iodine levels, which theoretically would benefit the thyroid gland by restricting the iodine the thyroid needs to produce its hormones.¹⁰ But it is a low protein, high carbohydrate, plant-based cat food which is inappropriate to feed to a cat whose dietary need for a high-quality, high-protein diet is critical.
Dr. Guillermo Díaz and family, including their four dogs (Leroy, Xica, Moza and Pepa) and six cats (Michalina, Tigger, Vladimir, Yellow, Mongo and Chirusa) moved to Buenos Aires, Argentina in July of 2017, where he expects to continue supporting different animal rescue groups, spread the benefits of raw food for cats and dogs and write articles about nutrition.
1. S. Kathleen Salisbury, DVM, MS, Diplomate ACVS, "Hyperthyroidism in Cats," Purdue University Continuing Education Article #3, Special Focus Feline Surgery, vol. 13, no. 9, North American Edition, Sept 1991.
2. Salisbury, "Hyperthyroidism in Cats."
3. Dye, Janice et. al. "Elevated PBDE Levels in Pet Cats: Sentinels for Humans?" Environmental Science and Technology, vol. 41, no. 18, September 15, 2007, 6350-6.
4. Carol Potera, "Chemical Exposures: Cats as Sentinel Species," Environmental Health Perspectives, vol. 115, no. 12, December 2007, A580.
5. CE Langston and NJ Reine, "Hyperthyroidism and the Kidney," Clinical Techniques in Small Animal Practice, vol. 21, no. 1, Feb 2006, 17-21.
6. ME Peterson, "Hyperthyroidism and Renal Disease: Is a 'Tapazole Trial' Necessary?" Insights into Veterinary Endocrinology, Nov 14, 2011.
7. Ellen S. Dierenfeld, PhD, Heather L. Alcorn, BS and Krista L. Jacobsen, MS, "Nutrient Composition of Whole Vertebrate Prey (Excluding Fish) Fed in Zoos," U.S. Department of Agriculture, May 2002.
8. AL Riis, JO Jørgensen, S Gjedde, H Nørrelund, AG Jurik, KS Nair, P Ivarsen, J Weeke and N Møller, "Whole Body and Forearm Substrate Metabolism in Hyperthyroidism: Evidence of Increased Basal Muscle Protein Breakdown," American Journal of Physiology, Endocrinology and Metabolism, vol. 288, no. 6, June 2005, E1067-73.
9. AH Sparkes, "Feeding Old Cats, An Update on New Nutritional Therapies," Topics in Companion Animal Medicine, vol. 26, no. 1, Feb 2011, 7-42.
10. Dr. Mark E. Peterson, Veterinary Endocrinologist, "Feeding Hill's y/d and Feline Immune Function," Insights into Veterinary Endocrinology.




